Case Report and Discussion
Arrhythmogenic cardiomyopathy (ACM), also known as arrhythmogenic right ventricular cardiomyopathy or dysplasia, is a rare genetically determined myocardial disease characterized by a fibrofatty replacement of the myocardium, predisposing the patient to life-threatening ventricular arrhythmias and sudden cardiac death (SCD) [
1]. ACM is associated with an increased risk of SCD particularly in young athletes and occasionally encountered in forensic practice [
2,
3].
Studies reveal the presence of inflammatory infiltrates in ACM specimens, suggesting a possible role of inflammation in the pathophysiology of the disease [
4,
5]. Although inflammation may be evidence of electrical instability that leads to ventricular tachycardia and SCD, the frequency, pattern, and severity of inflammatory infiltrates in ACM are variable, and the role of inflammatory cells remains under debate.
This autopsy case of a 52-year-old female aimed to highlight the importance of identifying inflammation in cases of ACM, with a literature review focused on inflammatory infiltrates.
The victim was a 52-year-old female, found unconscious in the morning at home by her husband, who called 119. In the emergency room, she was pronounced dead on arrival and reported to the police. According to her husband's statement, the patient complained of upper abdominal discomfort the night before death. Her medical history revealed that she had complained of frequent upper abdominal discomfort and hypotension during a regular health check three months prior. Her family history was unremarkable. Autopsy was performed on the day after death.
She was well-nourished. External examination revealed no injuries other than cardiopulmonary resuscitation and pricking finger's marks for alternative therapy. On internal examination, the heart weighed 400 g, and the anterior surface of the heart was diffusely covered with fatty tissue. On coronary artery examination, the left anterior descending branch showed focal severe atherosclerosis with 80% of luminal narrowing. Cross-section along the short-axis revealed diffuse fatty replacement on the free wall of the right (RV) and left ventricle (LV) and focal fatty ingrowth along the posterior wall of the LV (
Fig. 1). Both lungs were congested and edematous. The liver was found to be congested. Both kidneys exhibited slightly sclerotic surfaces. Other internal organs showed no specific findings.
Fig. 1.
Short-axis cross-section of the heart. Myocardium of the right ventricular free wall is diffusely replaced by fatty tissue. Left ventricle shows focal fatty ingrowth from the epicardial fat tissue in the posterior wall (arrow).

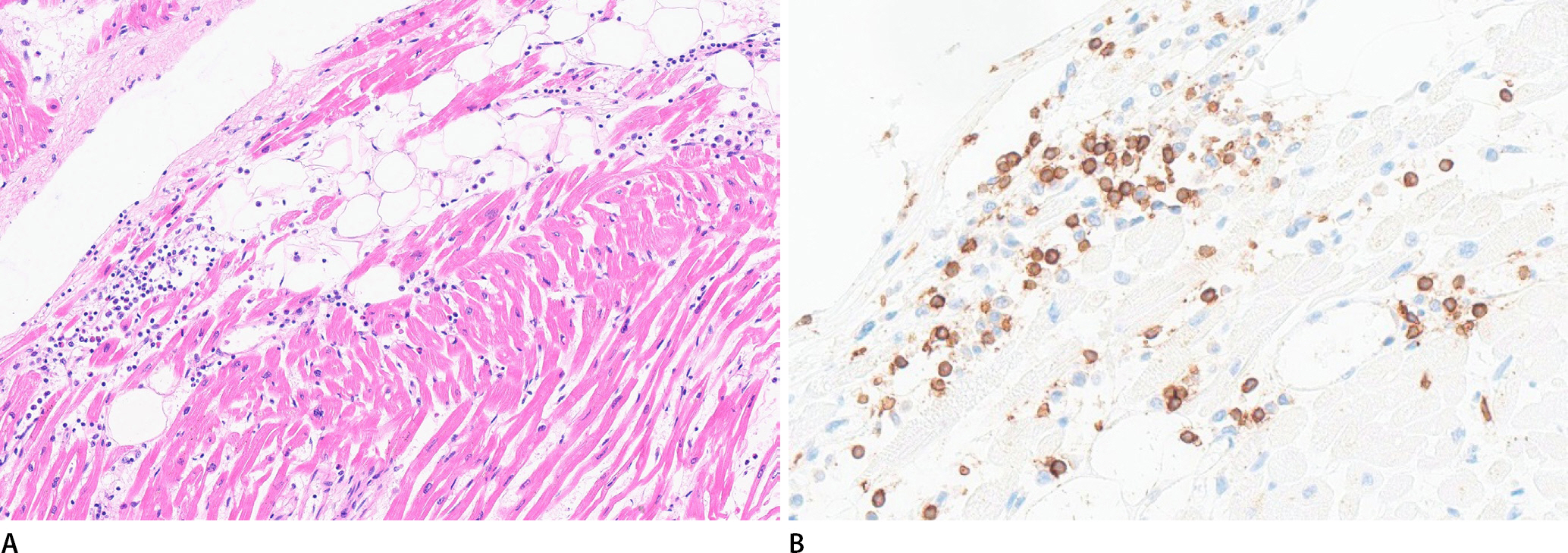
Microscopic examination of the RV revealed transmural replacement of the myocardium by fatty tissue and strands of atrophic myocytes, and the LV showed focal fatty ingrowth from the epicardial fat tissue along the posterior wall (
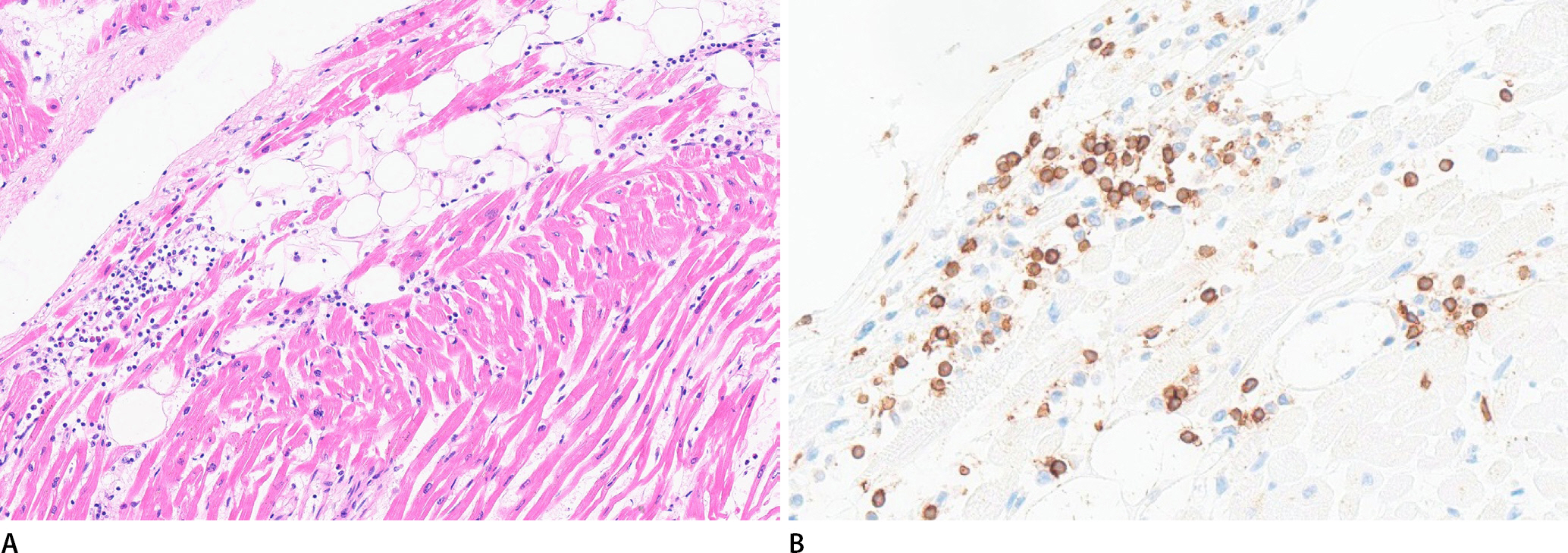
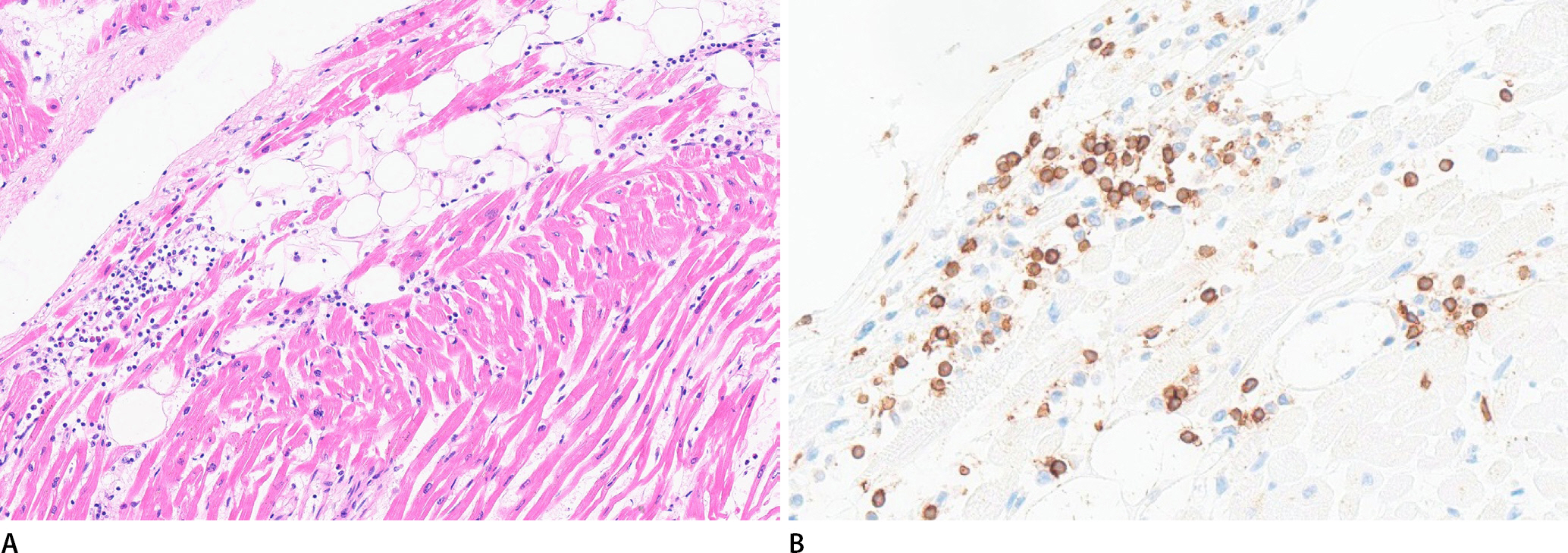
Fig. 2). Masson's trichrome staining of fatty replacements in both ventricles showed no definite collagen deposition between adipocytes. Inflammatory infiltrates and myocyte degeneration were prominent in the interstitium of the subendocardial layer adjacent to the fatty ingrowth of the LV (
Fig. 3A). The inflammatory cells mostly comprised CD3-positive lymphocytes, compatible with the immunohistochemical criteria of myocarditis (
Fig. 3B). Neutrophils, eosinophils, and macrophages were also observed. The severity of the inflammatory infiltrate varied in areas that were sparsely scattered and densely aggregated. Fewer lymphocytes were scattered between the atrophied myocytes compared than in the LV. No myocardial evidence of early ischemic injury due to coronary atherosclerosis was observed. Toxicological tests of the peripheral blood revealed no significant findings.
Fig. 2.
Microscopic finding of the right ventricle shows transmural fatty replacement of the myocardium with strands of atrophic cardiomyocytes (bottom: epicardial side) (H&E, ×40).

Fig. 3.
(A) Microscopic examination of the left ventricle shows interstitial infiltrate of lymphocytes, macrophages and eosinophils in the subendocardial layer adjacent to fatty ingrowth (H&E, ×200). (B) Interstitial infiltrate in the left ventricle is composed of mostly CD3-positive lymphocytes, thereby fulfilling the immunohistochemical criteria of myocarditis (CD3, ×400).
This case showed typical ACM pathology, predominantly involving the RV, and could be classified as a fatty variety based on the replacement tissue [
5]. In addition to the pathological hallmarks of ACM, inflammatory infiltrates in the myocardium were prominent in this case. Inflammatory infiltrates in ACM are reported in 32%-67% of cases, most severely in the subendothelial layers, more common in fibrofatty type and LV involvement cases [
4-
7]. The severity of inflammatory infiltrates is described in the literature as the presence of inflammatory cells or patchy infiltrates, some of which are compatible with the Dallas criteria for myocarditis [
4,
5]. Recently, the diagnosis of myocarditis is recommended to follow both histological and immunohistochemical diagnostic criteria, because non-specific inflammatory infiltrates in the myocardium is normally present [
8]. Inflammatory infiltrate in this case fulfills the immunohistochemical criteria of myocarditis using anti-CD3. One interesting point of this case is presence of prominent inflammatory infiltrate in this fatty variant while it is found mostly in fibrofatty variant. One reason of this difference seems to be due to different stage of inflammation because this case showed early active phase of inflammation with neutrophilic infiltrate noted, before the beginning of repair process and fibrosis.
Although the role of inflammation in ACM primarily caused by genetic defects in proteins of the cardiac intercalated disc is not entirely clear, it seems to be closely related to disease progression since different cardiotropic viruses were detected in sporadic cases and ACM-associated genetic variants were identified in some cases with acute myocarditis [
9,
10]. Inflammation could be a contributing factor directly to electrical remodeling and increased risk of arrhythmia because pro-inflammatory molecules generated during inflammatory process influence cardiac contractility [
9].
In the case of ACM, collecting multiple representative portions of cardiac tissue by the protocol for myocarditis is required to easily identify the cause of death and dying process since active inflammation may be associated with electrical instability predisposes the patient to life-threatening arrhythmias.