Introduction
Intracranial hemorrhage comprises of various types of hemorrhage as follows: epidural hemorrhage (EDH), subdural hemorrhage (SDH), subarachnoid hemorrhage (SAH), and intracerebral hemorrhage (ICH). These hemorrhages can be fatal. And natural or unnatural death is possible according to the type of intracranial hemorrhage. Deaths due to EDH and SDH may be unnatural and deaths due to ICH may be natural. Deaths due to SAH may be natural or unnatural. Furthermore, the identification and evaluation of the intracranial hemorrhage are essential during postmortem investigations such as postmortem inspection and autopsy, because deaths due to these hemorrhages are frequently objects of forensic autopsy [
1]. Previous reports showed that postmortem cisternal puncture can be useful to detect an intracranial hemorrhage [
2]. Postmortem cisternal puncture is usually conducted through the nuchal area and the cerebrospinal fluid (CSF) is aspirated from the cerebellomedullary cistern (CMC, known as the cisterna magna). However, the postmortem diagnosis of intracranial hemorrhage by postmortem cisternal puncture is limited because there are various types of intracranial hemorrhage. We assumed that it is impossible to identify all intracranial hemorrhages by cisternal puncture because blood may not exist in the CMC in some types of intracranial hemorrhage. Nowadays, postmortem computed tomography (PMCT) is used in many forensic medicine institutes worldwide and is recognized as a useful tool for postmortem diagnosis [
3]. In this study, we aimed to identify the hemorrhage in the CMC using PMCT in cases of various intracranial hemorrhage because CMC is a usual sampling site to identify blood for the postmortem diagnosis of an intracranial hemorrhage.
Materials and Methods
PMCT was performed before the autopsy. After the autopsy, the autopsy reports and PMCT were retrospectively reviewed. We found intracranial hemorrhage in 139 cases during the study period between August 2020 and July 2022. Of these, some were excluded to the following reasons: decomposed body (5 cases), excessive head injury (2 cases), postoperative (12 cases), and dental artifact (12 cases). Intracranial hemorrhage was categorized into EDH, SDH, SAH, and ICH. Furthermore, SAH cases were divided into basal and non-basal SAH.
PMCT images were obtained using a 160-channel multi-detector row computed tomography (CT) scanner (Aquilion Prime SP, Canon Medical Systems, Otawara, Japan). A whole-body scan was conducted for each subject in a supine position. Radiocontrast was not performed. Raw data was obtained with the following settings: 120 kVp, 215 mAs, 1.00 mm slice thickness, and 0.98 mm pixel size. The acquired PMCT images were restructured, and the resulting image data was imported into a 3D DICOM and Communications in Medicine workstation (Vitrea, Canon Medical Systems). After these procedures, the forensic pathologist confirmed the hemorrhage in the CMC. Hounsfield units (HUs) were measured at the normal brain parenchyma, hemorrhagic portion, and CMC using the aforementioned 3D DICOM software. Each region of interest (ROI) was set using 3D software, which semi-automatically calculated the similar HUs of the adjacent pixels. The workstation then automatically calculated the average density (HUs) in the ROI of the field and pixels. The authors double-checked both the ROI settings using 3D software and calculation of HUs by the workstation.
The P-values for continuous variables following normal distribution were derived from unpaired t-tests or one-way analysis of variance tests with subsequent Turkey's multiple comparison test. All statistical analyses were performed using the GraphPad Prism software (GraphPad Software, San Diego, CA, USA). Statistical significance was set at P<0.05.
Results
The autopsy cases of 76 men and 32 women were included. The age ranged from 2-86 years (average, 53.5 years). The number of cases of natural and unnatural deaths were 45 and 47, respectively. Among the natural deaths, there were 27 and 18 cases of ICH and basal SAH, respectively. Among the unnatural deaths, there were 1, 29, 2, and 15 cases of EDH, SDH, basal SAH, and non-basal SAH, respectively. The manner of deaths in the remaining 16 patients was undetermined. Among the 108 cases, the case number of main types of intracranial hemorrhage (EDH, SDH, SAH, and ICH) were 2, 40, 39, and 27, respectively. There were 21 and 18 cases of basal and non-basal SAH, respectively.
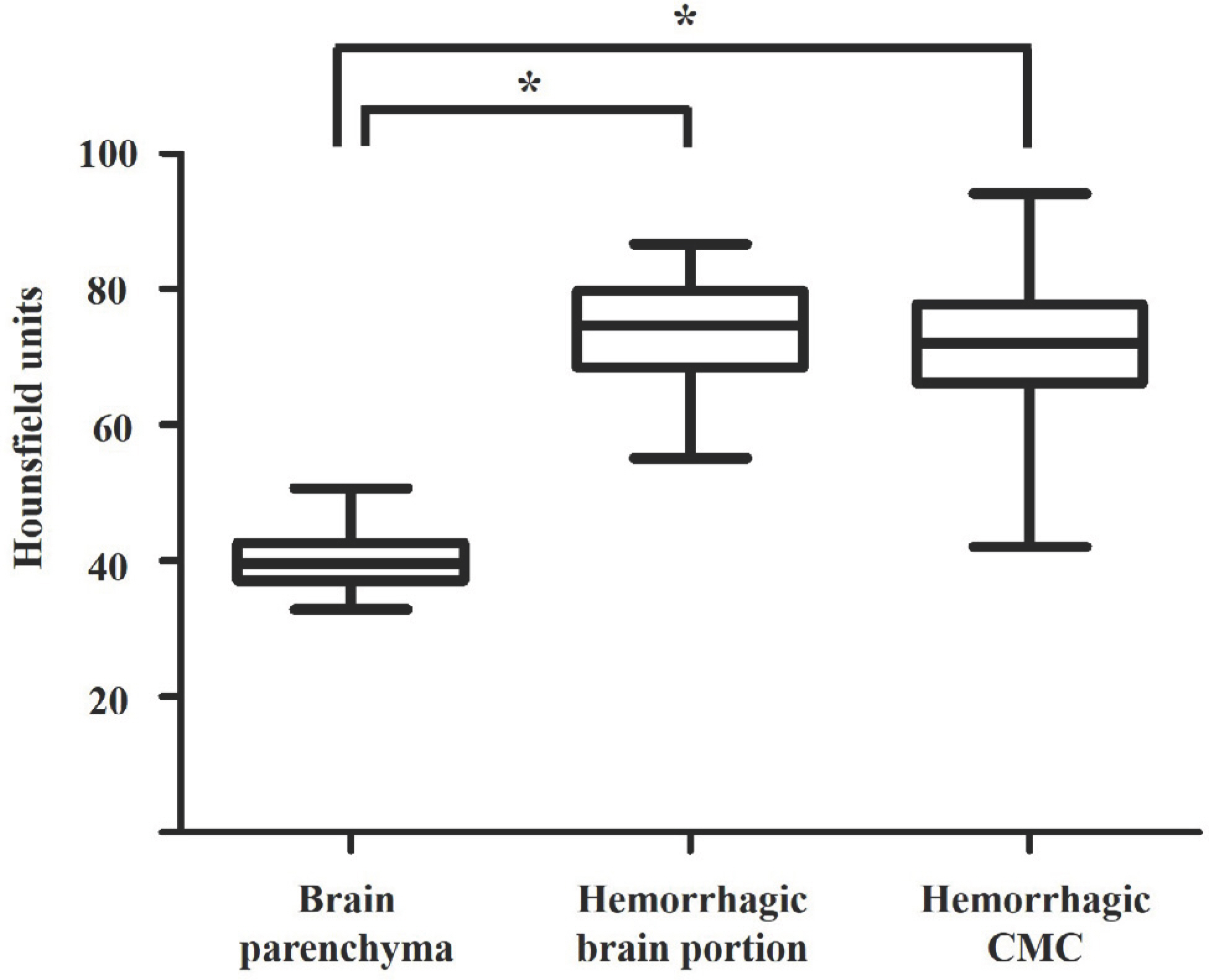
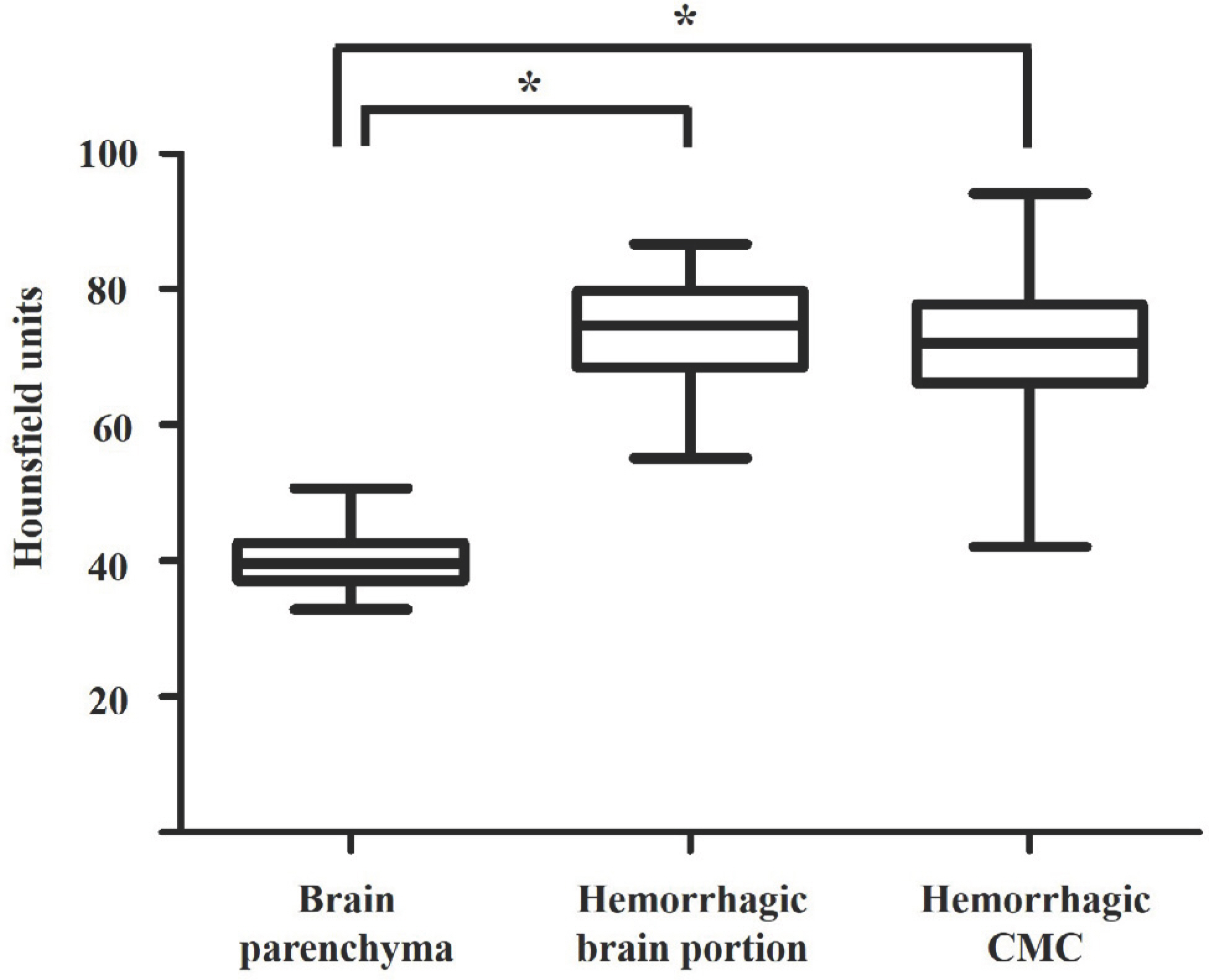
The PMCT density of the brain parenchyma was 40.1±4.6 HUs, whereas the hemorrhagic portion yielded a density measurement of 76.6±8.0 HUs (P<0.001) (
Fig. 1). Hemorrhage in the CMC was found in 42.6% (46/108) of the cases by PMCT and the PMCT density in the hemorrhagic CMC was 72.0±9.1 HUs (P<0.001) (
Fig. 2). Of the 46 cases with CMC hemorrhage, the HUs of the hemorrhagic brain portion and CMC were statistically different from those of the brain parenchyma (P<0.05) (
Fig. 3). Of the 46 cases with CMC hemorrhage, intracranial hemorrhages (EDH, SDH, basal SAH, non-basal SAH, and ICH) were 0, 7, 19, 9, and 11, respectively (
Table 1).
Fig. 1.
The Hounsfield units are statistically different between brain parenchyma and hemorrhagic brain portion in the 108 cases with intracranial hemorrhage.

Fig. 2.
Of 108 cases with intracranial hemorrhage, Hounsfield units of the cerebellomedullary cistern (CMC) are statistically different between non-hemorrhagic and hemorrhagic CMC.

Fig. 3.
Of the 46 cases with cerebellomedullary hemorrhage, Hounsfield units of hemorrhagic brain portion and cerebellomedullary cistern (CMC) were statistically different from that of the brain parenchyma. An asterisk indicates statistical significance (*P<0.05).
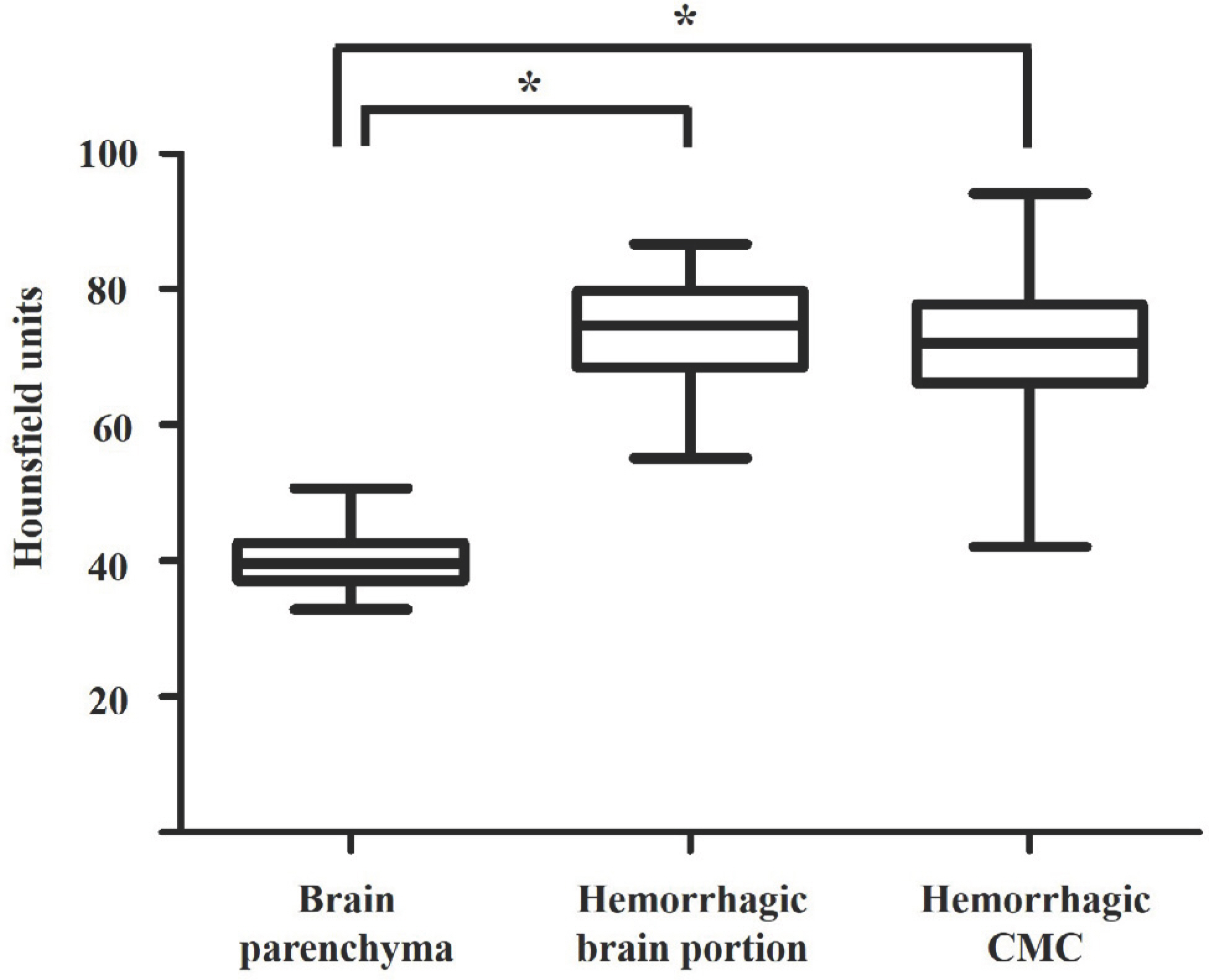
Table 1.
Hemorrhage in the CMC according to the type of intracranial hemorrhage
|
EDH |
SDH |
Basal SAH |
Non-basal SAH |
ICH |
|
Positive hemorrhage in the CMC |
0 |
7 (17.5) |
19 (90.5) |
9 (50.0) |
11 (40.7) |
|
Negative hemorrhage in the CMC |
2 (100) |
33 (82.5) |
2 (9.5) |
9 (50.0) |
16 (59.3) |
|
Total |
2 |
40 |
21 |
18 |
27 |
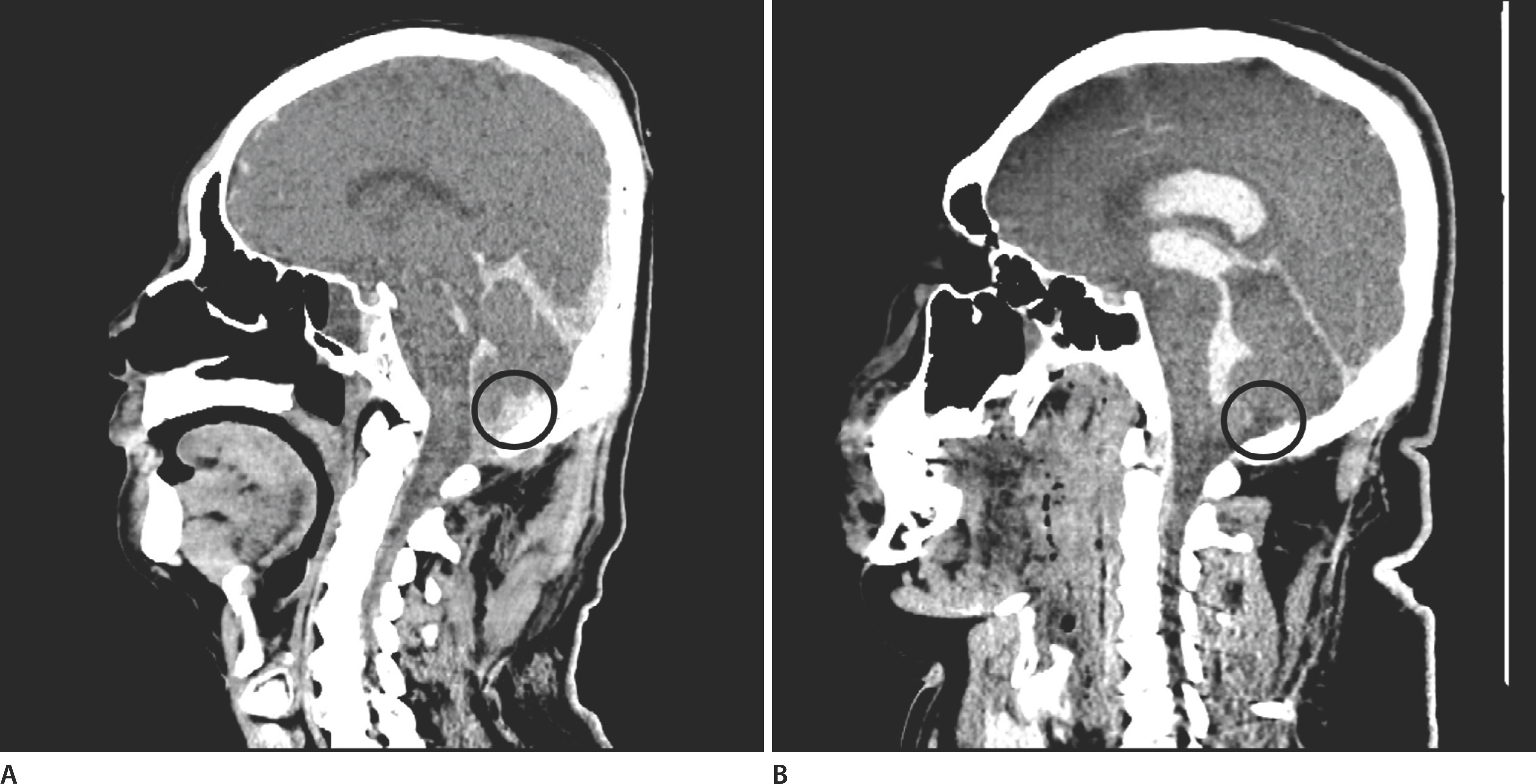
Hemorrhage in the CMC was not identified in the two EDH cases. Hemorrhage in the CMC was identified in seven of the 40 SDH cases (17.5%), and of them (seven cases), hemorrhage such as SAH and intraventricular hemorrhage (IVH) was combined in five cases. Location of SDH was near the CMC in the remaining two cases. In 19 of the 21 cases (90.5%) with basal SAH, hemorrhage in the CMC was identified using PMCT. There were three cases of traumatic basal SAH, of them, hemorrhage in the CMC was not identified in the one case. Of the 18 cases of non-basal SAH, hemorrhage in the CMC was identified in nine cases. These cases showed a tendency toward a large SAH, and four cases were combined with IVH. Among cases of SAH, there were cases with no blood in the CMC by PMCT (
Fig. 4). Hemorrhage in the CMC was identified in 11 of the 27 patients (40.7%) with ICH, and hemorrhages such as SAH and IVH were combined in 10 patients (
Table 1).
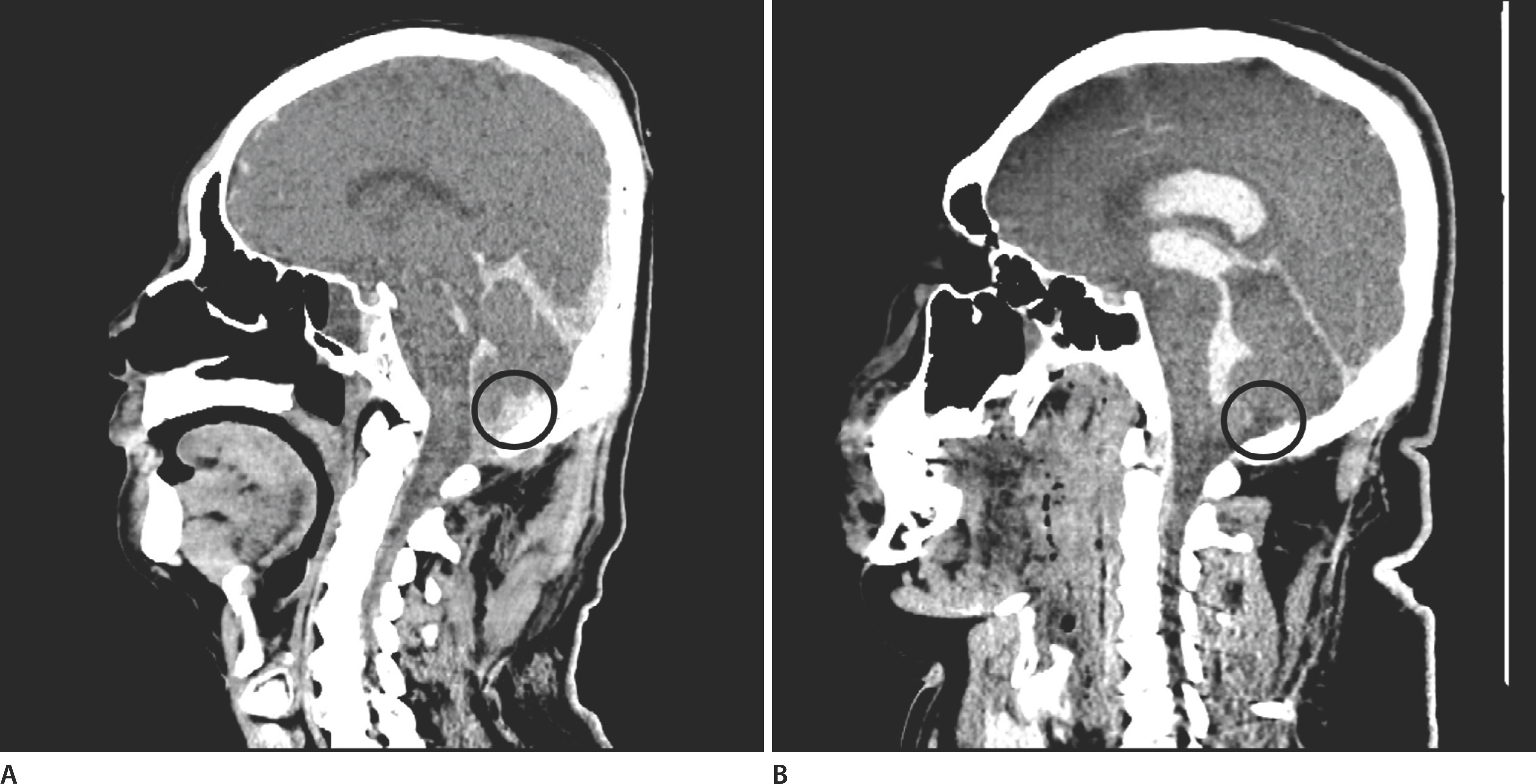
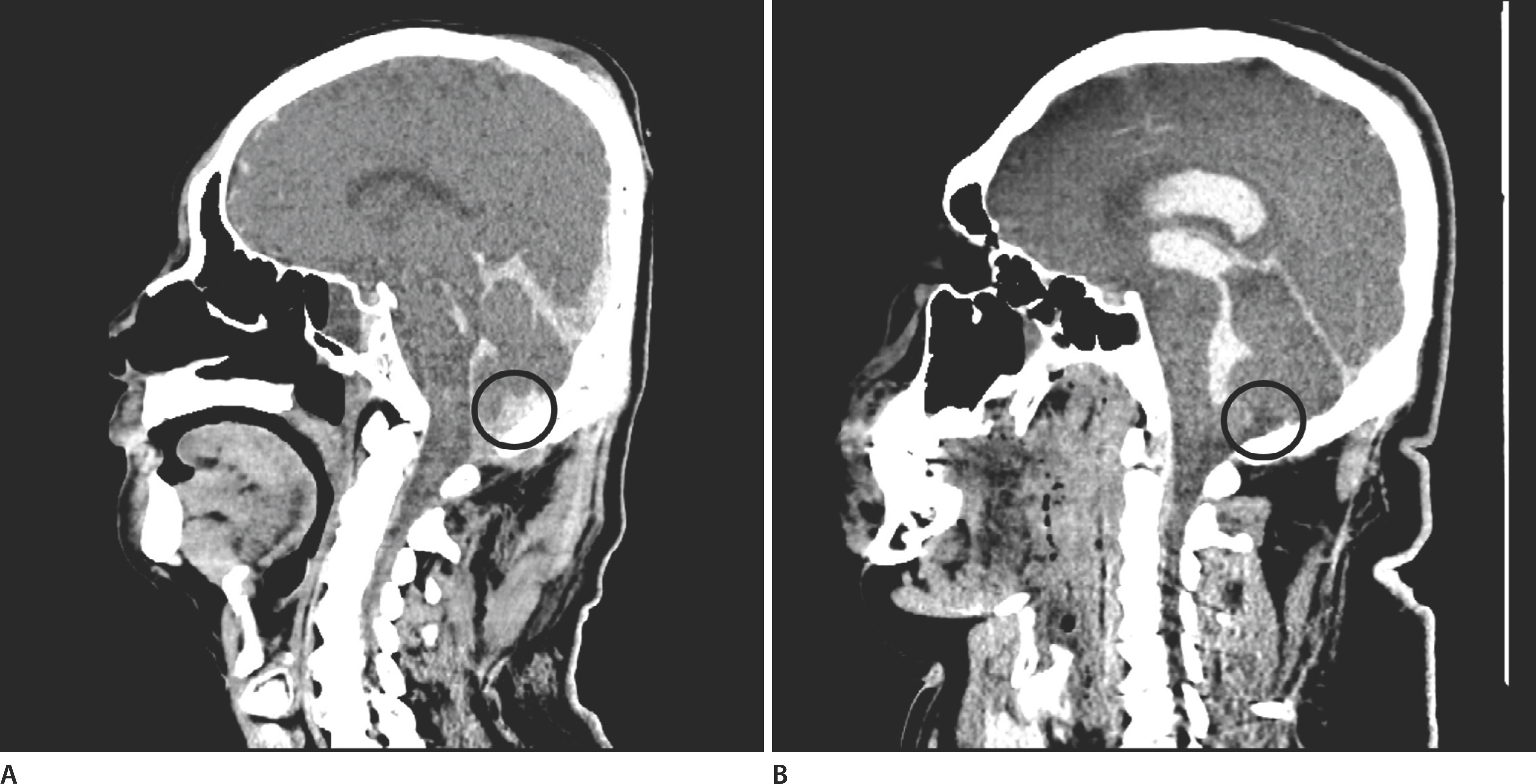
Fig. 4.
Sagittal plane of postmortem computed tomography shows blood in the cerebellomedullary cistern (CMC) in the case of subarachnoid hemorrhage. An average Hounsfield unit is 60.1 in the hemorrhagic CMC region (A). There is no blood in the CMC due to obstruction of the median and lateral apertures in this case of subarachnoid and intraventricular hemorrhage. An average Hounsfield unit is 12.5 in the non-hemorrhagic CMC region (B). A black circle indicates the CMC.
Discussion
Currently, PMCT is widely used in many forensic institutes. Reconstruction of CT images is performed mathematically from a large amount of X-ray projection data acquired at many different angles of the plane. This information regarding the voxels is translated into a relative measure of radiodensity, known as the CT number or HU. Acute hemorrhage exhibits a higher density than brain parenchyma on non-contrast CT images taken before or after death because of the high protein concentration (mainly globin molecules) in the blood [
4]. The average HU was 76.6 points for intracranial hemorrhage in this study, and we could regard foci above 60 HUs as a hemorrhage. Furthermore, we could regard foci <40 HUs as a no hemorrhage. The foci between 40 and 60 HUs were borderline [
5]. PMCT is particularly useful for detecting intracranial hemorrhage in forensic medicine. In previous studies, pre-autopsy PMCT accurately detected intracranial hemorrhage in highly decomposed bodies [
6,
7]. And PMCT was reported to be more useful than clinical diagnosis for identifying the immediate cause of death in hospitalized patients not undergoing autopsy [
8]. In this study, we analyzed the presence of blood in the CMC using PMCT among various intracranial hemorrhage cases confirmed by conventional autopsy.
Death due to EDH is rare in forensic autopsy cases, and CMC hemorrhage was not identified by PMCT in this study. Blood in the EDH is located between the skull and the dura mater, and the major site of EDH is the temporal area. Therefore, we believe that our results are acceptable. SDH was the most common intracranial hemorrhage in this study (40/108). Blood in the SDH is located between the dura and the arachnoid mater. However, blood can exist in the subarachnoid space when the thin arachnoid mater is broken. Hemorrhage in the CMC was identified in seven of 40 cases (17.5%) with SDH in this study. Hemorrhage in CMC was most frequently identified in cases of basal SAH (90.5%). Blood in basal SAH is located in the subarachnoid space and can be mixed with CSF; the location of hemorrhage in basal SAH is close to the CMC. In contrast, CMC hemorrhage was identified in 50% of non-basal SAH. The location of the hemorrhage can be far from the CMC in non-basal SAH cases, and coagulated blood can obstruct narrow points such as the cerebral aqueduct of Silvius, which connects the third and fourth ventricles and the median and lateral apertures that connect the fourth ventricle and the CMC. Blood can extend into the adjacent ventricle in ICH when hemorrhagic brain parenchyma is destroyed. CMC hemorrhage was identified in 40.7% of ICH cases using PMCT.
This study has some limitations. Hemorrhage detection in the CMC by PMCT was hindered by several factors: dental artifact, severe head trauma such as crashed skull fracture including skull basal fracture, postoperative state, and advanced brain edema. Normal postmortem changes in the brain include loss of gray-white matter differentiation and brain swelling with effacement of ventricles and cisterns, beginning immediately after death. Furthermore, the normal postmortem changes significantly affect the extent and imaging characteristics of SDH [
9] and PMCT including postmortem sampling was suggested to be used as an adjunct rather than a substitute to autopsy [
10,
11].
Although CSF sampling through cisternal puncture is recommended as a part of postmortem examination [
12], false-positive results can be achieved by traumatic tapping during cisternal puncture. The results of this study did not guarantee the usefulness of postmortem cisternal puncture in identifying intracranial hemorrhage during postmortem investigation. Nevertheless, this study highlights several significant findings. This study verified hemorrhage in the CMC according to various intracranial hemorrhages using PMCT and showed its possibilities and limitations.