Case Report and Discussion
Fat embolism (FE) and fat embolism syndrome (FES), the formation of fat droplets in the circulating blood due to trauma or non-traumatic causes, can block small arteries and capillaries of organs, especially the lungs (pulmonary fat embolism). Symptoms of FES vary according to the degree of FE. The onset of pulmonary symptoms (such as dyspnea, cyanosis, chest pain, and cough) and the brain (such as insomnia, memory loss, delirium, and coma) can occur within 12-72 hours after injury, and can be fatal in severe cases [1]. Damage to long bones or adipose tissue is the most common cause of FE. Bone damage, including fracture, contusion, orthopedic surgery or treatment, and damage to adipose tissue, can be caused by extensive subcutaneous trauma. Rare but non-traumatic causes, like alcoholic liver disease, pancreatitis, severe burns, frostbite, and adrenal cortical treatment, have also been reported [2]. Herein, we report a case of sudden death due to FES and describe its clinical implications and the pathological findings.
A 79-year-old man was hit by a car while crossing a crosswalk. The victim was then immediately transferred to the emergency department. Computed tomography (CT) of the lower extremities confirmed an intertrochanteric fracture of the right femur. Brain, abdomen, and chest CT, and echocardiography performed preoperatively in the emergency room showed no abnormal findings. He had hypertension and stroke as underlying diseases and was taking aspirin; however, the blood coagulation test showed normal ranges before the surgery. The initial blood test revealed a white blood cell count of 6,000/mm┬│, a hemoglobin level of 11.6 g/dL, and a platelet count of 179,000/mm┬│. Twenty-three hours after trauma, closed reduction and internal fixation surgery were performed under general anesthesia to treat the fracture. However, during the final stage of surgery (suturing), his systolic blood pressure dropped to 50 mmHg and the mental state deteriorated to a drowsy state. His body temperature measured over 39┬░C and the pulse rate was over 130 beats/min. Cardiopulmonary resuscitation was performed to restore spontaneous circulation. Despite management, the patients died 4 hours after surgery, 27 hours after the trauma. At the time of death, blood tests showed a leukocyte count of 11,200/mm┬│, a hemoglobin level of 8.0 g/dL, and a platelet count of 49,000/mm┬│. Arterial blood gas analysis conducted during mechanical ventilation revealed hypoxia, with a PaO2 of 72 mmHg and a PCO2 of 52 mmHg.
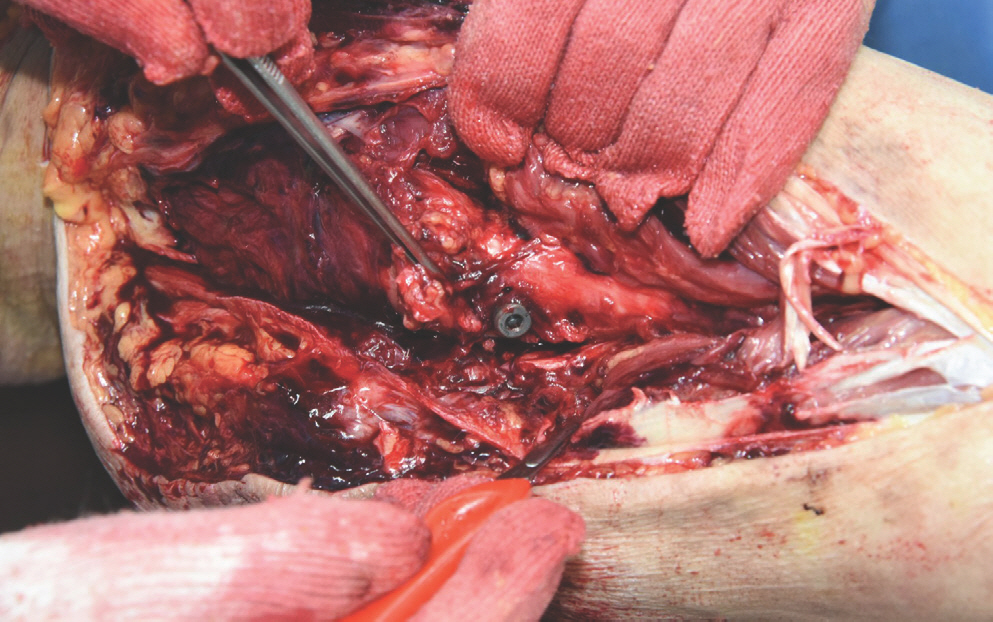
An autopsy was performed 3 days after death. The deceased had a height of approximately 158 cm. Livor mortis was present as a reddish-purple discoloration on the back. External examination revealed no petechiae in his conjunctiva, and metal fixation of a right fractured femoral region approximately 2.5 cm long was observed (Fig. 1). An internal examination revealed moderate atherosclerosis in the branches of the major coronary arteries.
Fig.┬Ā1.
Right femur intertrochanteric fracture with closed reduction and internal fixation surgery.
Toxicology testing of the blood and gastric contents of the deceased showed no specific findings, except for the presence of anesthetic drugs (propofol and lidocaine) and analgesic drugs (tramadol), which were within the acceptable therapeutic levels. The blood alcohol concentration was less than 0.010%.
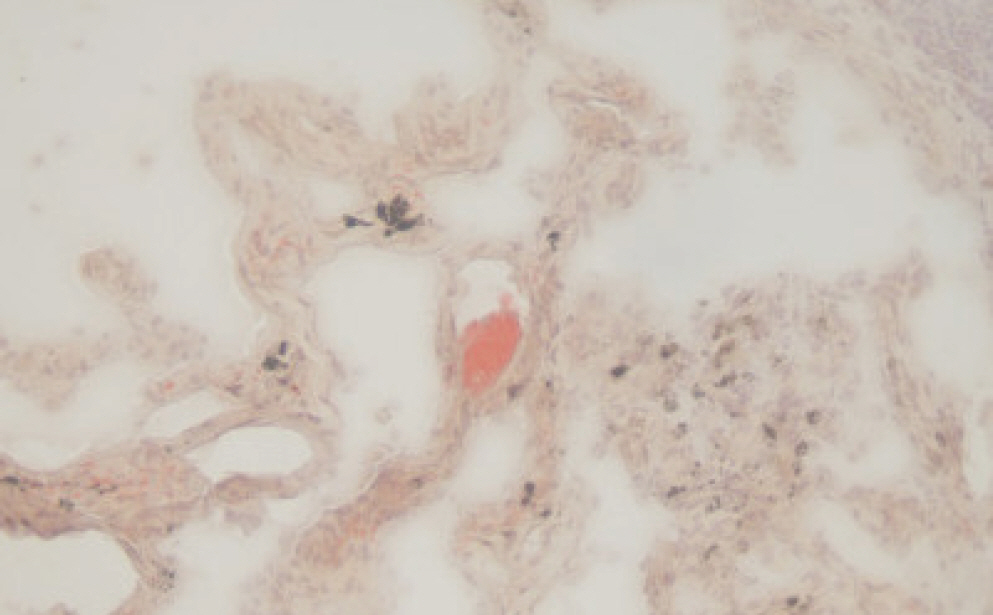
Histological examination revealed a few fat droplets in the pulmonary capillaries (Fig. 2). To confirm the FE, the lung tissue was cryo-sectioned and stained with Oil Red O, which revealed sporadic red-stained fat droplets (Fig. 3).
Fig.┬Ā2.
H&E stained section of lung, showing sporadic fat droplets within the pulmonary microvasculature (├Ś200).
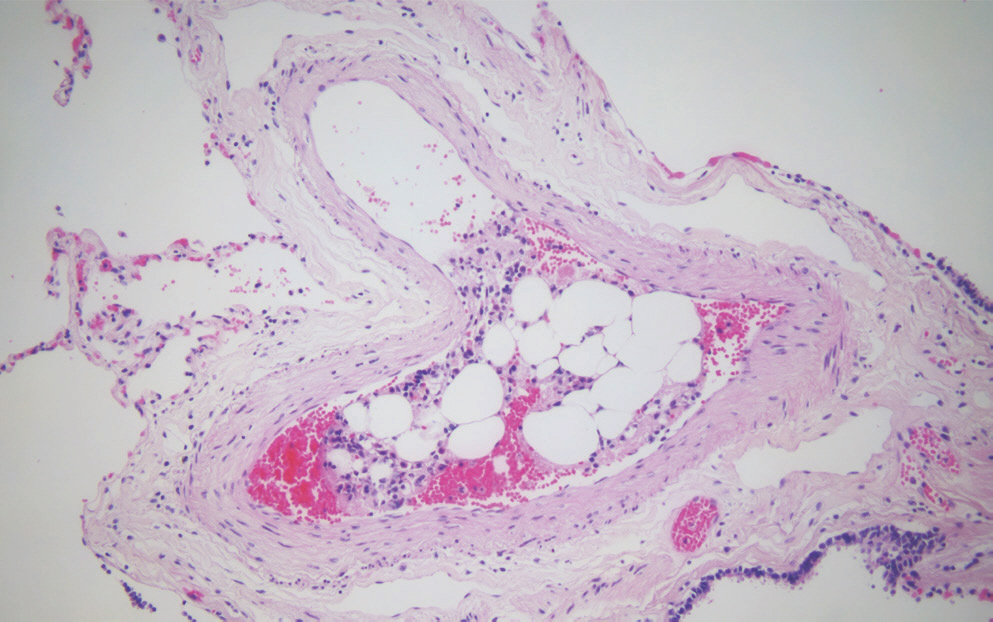
Fig.┬Ā3.
Oil Red O stained section of frozen lung tissue, showing sporadic red-stained fat droplets within the pulmonary microvasculature (├Ś400).
Although atherosclerosis was observed in the coronary arteries, it was excluded as a cause of death based on the clinical course. Given that the preoperative hemoglobin level and vital signs were within the normal range, and no intra-abdominal bleeding was noted during the autopsy, hypovolemic shock was also ruled out as the cause of death. Therefore, FES was diagnosed as the cause of death, considering both the autopsy findings and the clinical course and we determined manner of death of this case as accident.
FE is characterized by blockage of blood vessels by fat particles. The condition predominantly occurs in association with traumatic injuries and potentially affects >90% of patients with long bone fractures, with a mortality rate reported as 5%-20% [3]. On the other hand, the mortality rate associated with FES was previously reported to be 10%-20% until the 1970s. Recent studies have suggested a decrease in mortality, with rates ranging from 5%-10% [4,5].
Respiratory symptoms such as difficulty in breathing and bluish discoloration of the skin (cyanosis) typically precede the onset of FES. These systemic symptoms manifest in approximately 75% of patients. Central nervous system symptoms, including headache, drowsiness, confusion, seizures, and coma, were the second most common set of symptoms. Skin petechiae, small red or purple spots typically found on the chest, neck, armpits, oral mucosa, and conjunctiva, have been reported in 50%-60% of cases. These petechiae usually resolve within 1 week [3].
According to the criteria proposed by Gurd and Wilson for FES (Table 1), for diagnosis, the presence of at least two major criteria or one major criterion, along with four minor criteria, is essential. The three major criteria are respiratory failure, altered consciousness, and skin petechiae. There are also nine minor criteria: fever (usually below 39┬░C), tachycardia (heart rate over 120 beats/min), retinal abnormalities, jaundice, renal abnormalities (such as anuria or oliguria), anemia (a decrease of more than 20% in hemoglobin levels from admission), thrombocytopenia (platelet count reduced by more than 50% from admission), elevated erythrocyte sedimentation rate of more than 71 mm/hr, and presence of fat macroglobulinemia [6]. In the present case, the deceased exhibited two major symptoms (hypoxemia and altered consciousness) and four minor symptoms (fever, tachycardia, anemia, and thrombocytopenia). Based on these criteria, FES was clinically diagnosed.
Table┬Ā1.
Gurd and Wilson's diagnostic criteria for FES
Falzi et al. (1964) [7] proposed a classification system for quantifying the histological grade of FE based on the characteristics of fat droplets. According to their classification, the grades are as follows: grade 0ŌĆö not FE (punctiform when presentŌĆösporadic and not in every microscopic field); grade 1ŌĆölight FE when the form of embolism was described as drop-shaped and sporadic in every microscopic field; grade 2ŌĆöwhen multiple, disseminated in every microscopic field and sausage-shaped or rounded; and grade 3ŌĆöwhen antler shaped and numerous everywhere, in every microscopic field [7]. In the present case, we observed sporadic fat droplets microscopically (two 200├Ś fields) during the histological examination of the lungs, indicating grade 0 FE. Nevertheless, based on Gurd's criteria, the clinical findings were consistent with a diagnosis of FES. Therefore, FES was defined as the cause of death.
As FE/FES has fatal outcomes, it leads to many legal problems, including lawsuits. FE/FES occurs unexpectedly, and when such patients show a rapid clinical course during medical treatment, many lawsuits are filed against the medical staff for compensation for damage or professional negligence as a manslaughter. For example, for a victim who fell alone on the street, thigh fracture surgery was performed under spinal anesthesia 3 days after the injury. One hour postoperatively, the patient experienced chest pain and respiratory distress. Cardiopulmonary arrest occurred 4 hours after surgery, and the victim died 5 hours after surgery. A lawsuit for compensation for damages was filed against the medical staff. However, the court dismissed the plaintiff's claim in the lawsuit because FE is difficult to predict even in clinical practice; there was virtually no other treatment other than oxygen administration for FE, and the medical staff seemed to have taken appropriate measures as medical standards [8].
Although many studies are being conducted on FES, diagnosing FES remains a big challenge. Defining Gurd and Wilson's diagnostic criteria as the gold standard is difficult because they rely on the comprehensive observation of clinical features rather than a specific test [9]. However, it can be understood as a screening standard that raises awareness about FES in clinical practice and discriminates against various diseases, including FES.
We report a case of fat droplets appearing as grade 0, which can be easily overlooked when artifacts are considered. However, it is important to closely examine medical records in the clinical course when FES may occur, and regardless of the amount of fat droplets, FES should not be ignored.