Death from Malignant Transformation of Untreated Mucinous Borderline Tumor: Case Report
Article information
Trans Abstract
Mucinous borderline tumors (MBT) of the ovary with mild to moderately atypical epithelial cells that produce mucin rarely recur and very rarely become malignant after surgery. Due to their low malignant potential and large tumor size, most cases are diagnosed in stage I and have a good prognosis. The authors reported a case of MBT, which had been left untreated after diagnosis, progressed to stage IV, and caused massive pleural effusion (>3,000 mL) resulting in death. Grossly, severe abdominal swelling, a huge multiloculated cystic mass in the left ovary, and a metastatic mucinous mass in the pleura and peritoneum were observed. Histological findings include gastrointestinal type epithelial cells with mucin secretion, degenerative and autolytic nuclei, and occasional infiltration of inflammatory cells. Because sufficient sections cannot be made according to the clinical pathology criteria in forensic autopsy, efficient decisions are required during autopsy for diagnosis.
Discussion
A mucinous borderline tumor (MBT) is an ovarian tumor with a low malignant potential and good prognosis. The authors report a case of autopsy in an untreated patient with MBT. The deceased was a 39-year-old woman who had several mental disorders, including chronic alcoholism, and lived alone away from her family. Her abdomen had been swollen for 2 years before she died. One year before her death, her abdomen was similar in appearance to that of a pregnant woman. Her body was found in the men's restroom of a commercial building at dawn.
Post-mortem inspection revealed severe abdominal swelling (Fig. 1A), pitting edema in the lower extremity, and a few petechiae of the conjunctivas without trauma. Because a detailed clinical history was not revealed, forensic inspectors suggested the possibility of pregnancy, or ascites-related chronic alcoholic liver cirrhosis. In addition, a medical examiner proposed the possibility of a malignant tumor of unknown origin.
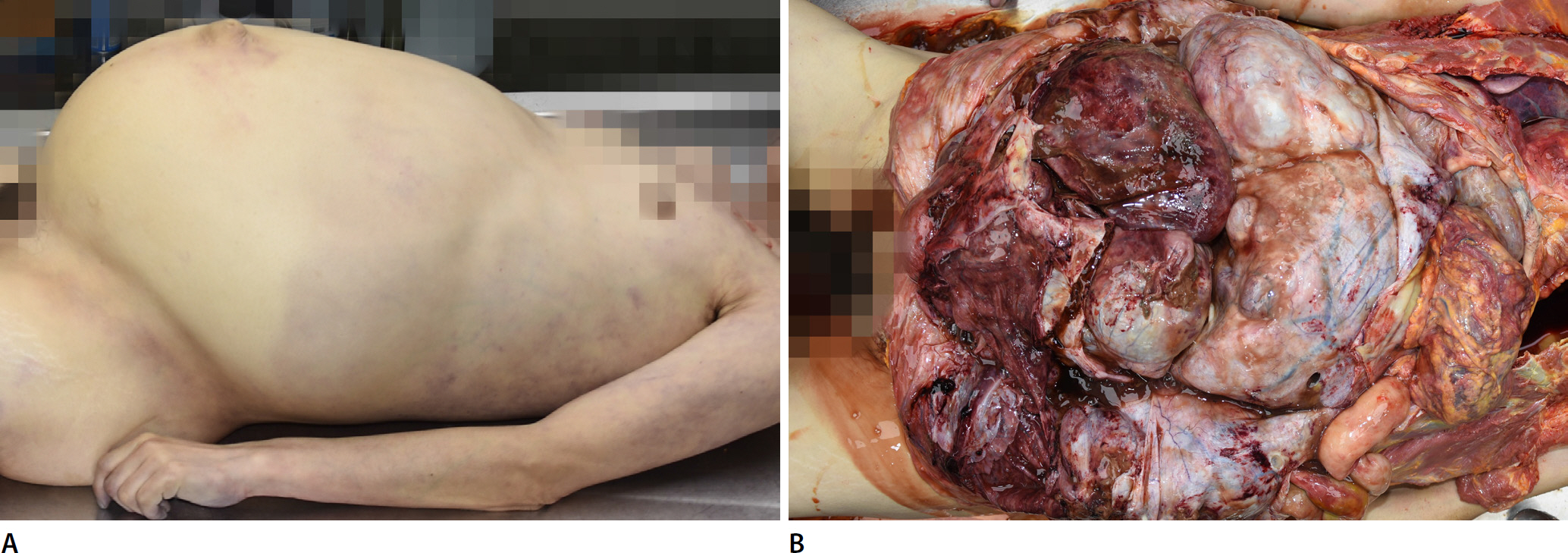
(A) Severe abdominal swelling. (B) Bulging out multiloculated cystic mass occupying the whole abdominal cavity.
Autopsy was performed the day after the woman's body was found. In the abdominal cavity, the greater omentum was fibrotic and thickened. Under the greater omentum, a huge multiloculated cystic mass measuring approximately 36×25×15 cm was observed (Fig. 1B). The cut surface was filled with a mucinous fluid. Solid lesions were not observed. The cystic mass was not adherent to the peritoneum or other organs and was connected to the left salpinx. Therefore, we believe that it originated in the left ovary. The right ovary was intact. Ascitic fluid was measured >2,700 mL. There were many small mucinous nodules in the retroperitoneum and mesocolon of the sigmoid colon (Fig. 2A). In the thoracic cavity, left pleural effusion measuring >3,000 mL caused severe deviation of the heart and atelectasis of the left lung (Fig. 2B). A metastatic mass was not observed in the parenchyma of either lung. However, a diaphragmatic mucinous mass measuring 4×3×3 cm was observed (Fig. 2C).
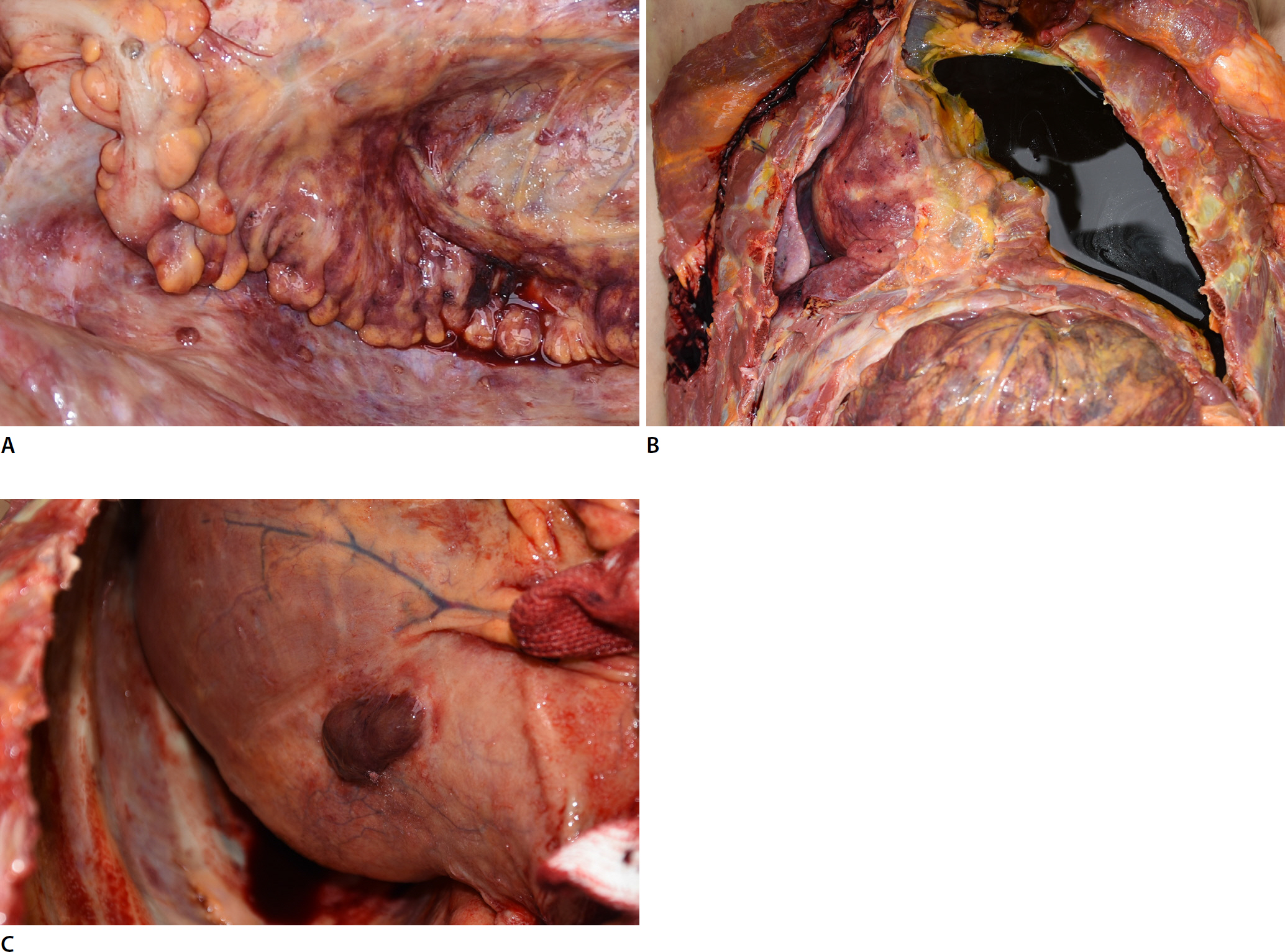
(A) Several small mucinous nodules in the retroperitoneum and mesocolon of the sigmoid colon. (B) Massive left pleural effusion (> 3,000 mL) causing severe rightward deviation of the heart and atelectasis of the left lung. (C) A mucinous mass in the diaphragm (size, 4×3×3 cm).
Toxicological analysis results were negative. Histologic examination of ovarian tumors revealed multiloculated cysts with gastrointestinal epithelial cells secreting mucin and extracellular mucin pools (Fig. 3A). Each tumor cell was separated, lost cohesiveness, and had an autolytic nucleus. In a few foci, variable inflammatory infiltrates, including neutrophils and macrophages, were observed (Fig. 3B). However, these findings were insufficient to be considered definite necrosis of tumor cells. In several sections, findings suggesting malignancy, such as microinvasion, intraepithelial carcinoma, and mural nodules, were absent.
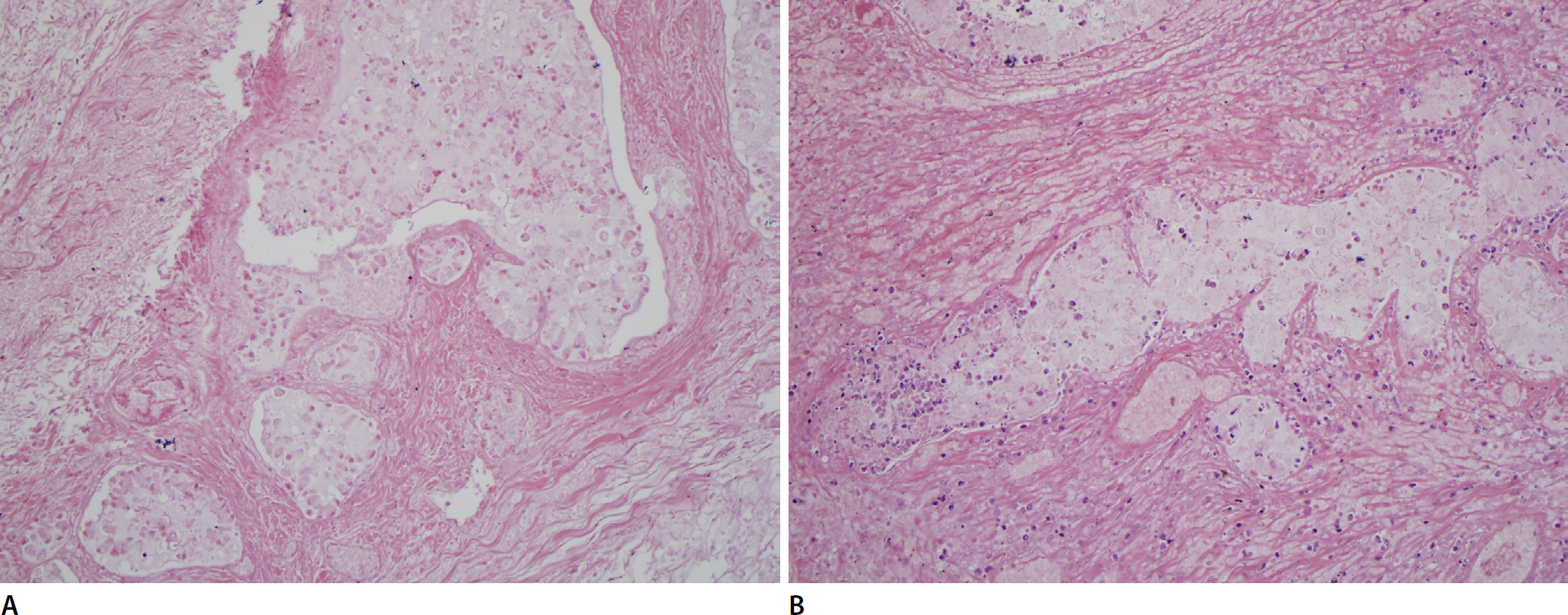
(A) Multilocular cyst lined by gastrointestinal mucinous epithelial cells with extracellular mucin pools. (B) Loosely cohesive tumor cells with autolytic nucleus. This field shows variable inflammatory infiltrates including neutrophils and macrophages (A and B, H&E, ×200).
In summary, this large ovarian mass was a mucinous cystic tumor without malignant findings but with pleural and peritoneal metastases. Therefore, it is proposed that untreated MBT progressed to malignant transformation and finally attained the metastatic ability to become a stage IV disease. In conclusion, the cause of death is a cardiopulmonary function disorder caused by massive pleural effusion and ascites from metastatic nodules of ovarian tumors.
MBT is a mucinous ovarian tumor with mild to moderately atypical mucin-containing epithelial cells [1]. The largest tumor size is several centimeters to 50 cm [2]. Because most cases are diagnosed in stage I (96.2%), the prognosis is good, and patients in advanced stages are very unusual [3]. After oophorectomy, 11% of patients experience recurrence and 20%-30% of recurrent cases show malignant transformation [4]. Therefore, death among patients with MBT who have been followed up has rarely been reported [5].
This case shows how MBT could progress for more than 2 years. According to an additional investigation, the deceased was diagnosed with MBT at the university hospital and an operation schedule was established. However, she did not undergo surgery for an ovarian tumor. Although MBT has low malignant potential, if not treated surgically, it can cause death due to complications rather than aggressive invasion of the tumor.
We grossly observed metastatic mucinous masses in the pleura and peritoneum, but no definite histopathological findings were confirmed. Due to the conditions of the autopsy room in Korea, it is difficult to make enough sections of the ovarian tumor and all metastatic masses. For the accurate histopathological diagnosis of ovarian tumors, one section per centimeter of the largest tumor dimension is recommended [6]. Furthermore, the quality of autopsy specimens is worse than that of surgical specimens owing to degeneration by autolysis and putrefaction. Considering the above pathological recommendation and the poor quality of the specimen, more than 50 sections were needed in this case. Since pathologically accurate diagnosis is difficult in forensic autopsy, it is necessary to consider a standard procedure for forensically efficient diagnosis of tumors similar to ovarian tumors. Above all, the practical decision of the medical examiner is important in autopsy.
Notes
Conflicts of Interest
Jinhyuk Choi, a contributing editor of the Korean Journal of Legal Medicine, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Acknowledgments
Special thanks to Yoo Hoon Kim and Yikyeong Chun for the advice and help they provided during the writing of this paper.
