1.Mocchegiani R, Nataloni M. Complications of infective endocarditis. Cardiovasc Hematol Disord Drug Targets 2009;9:240-8.


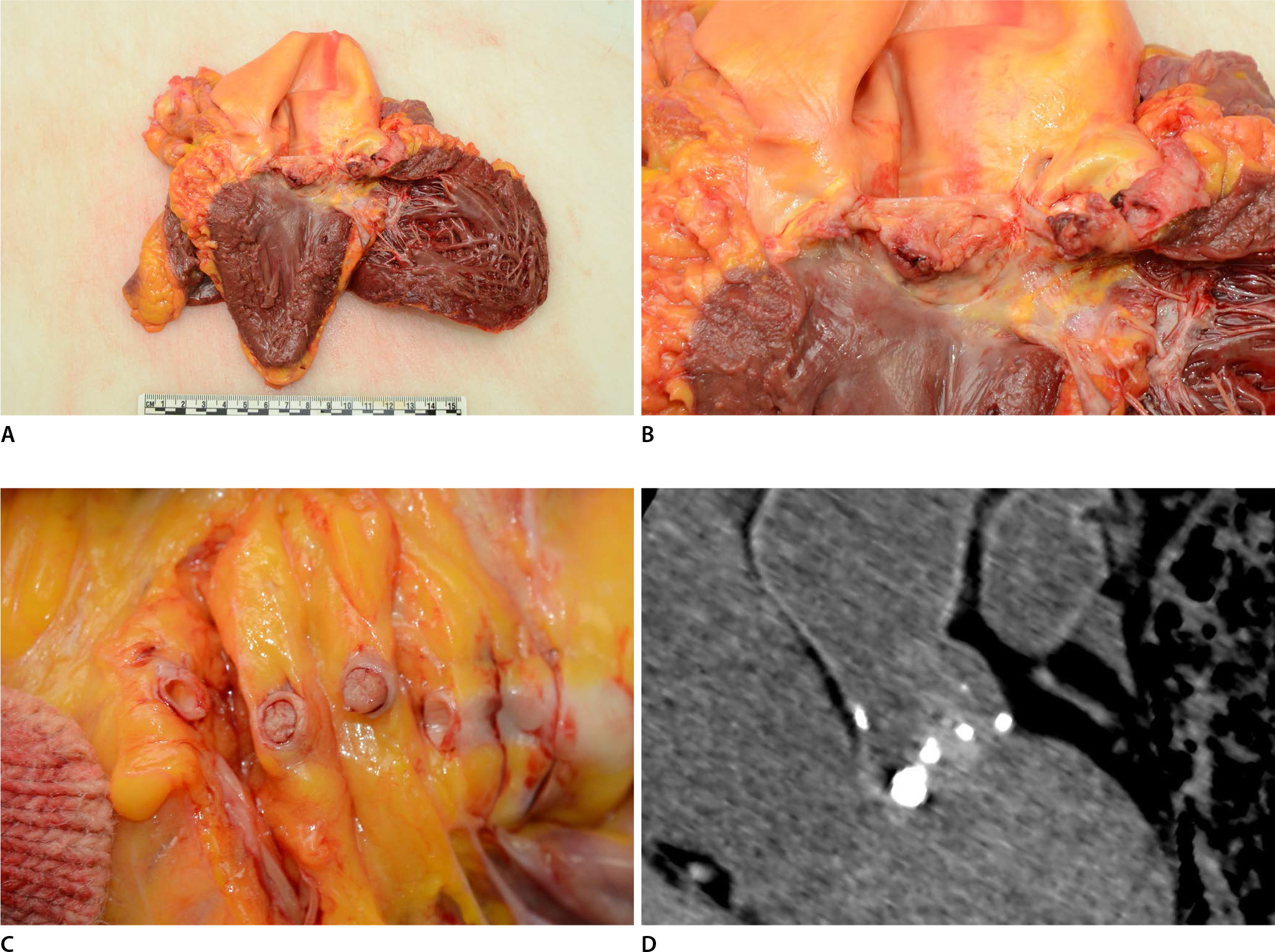
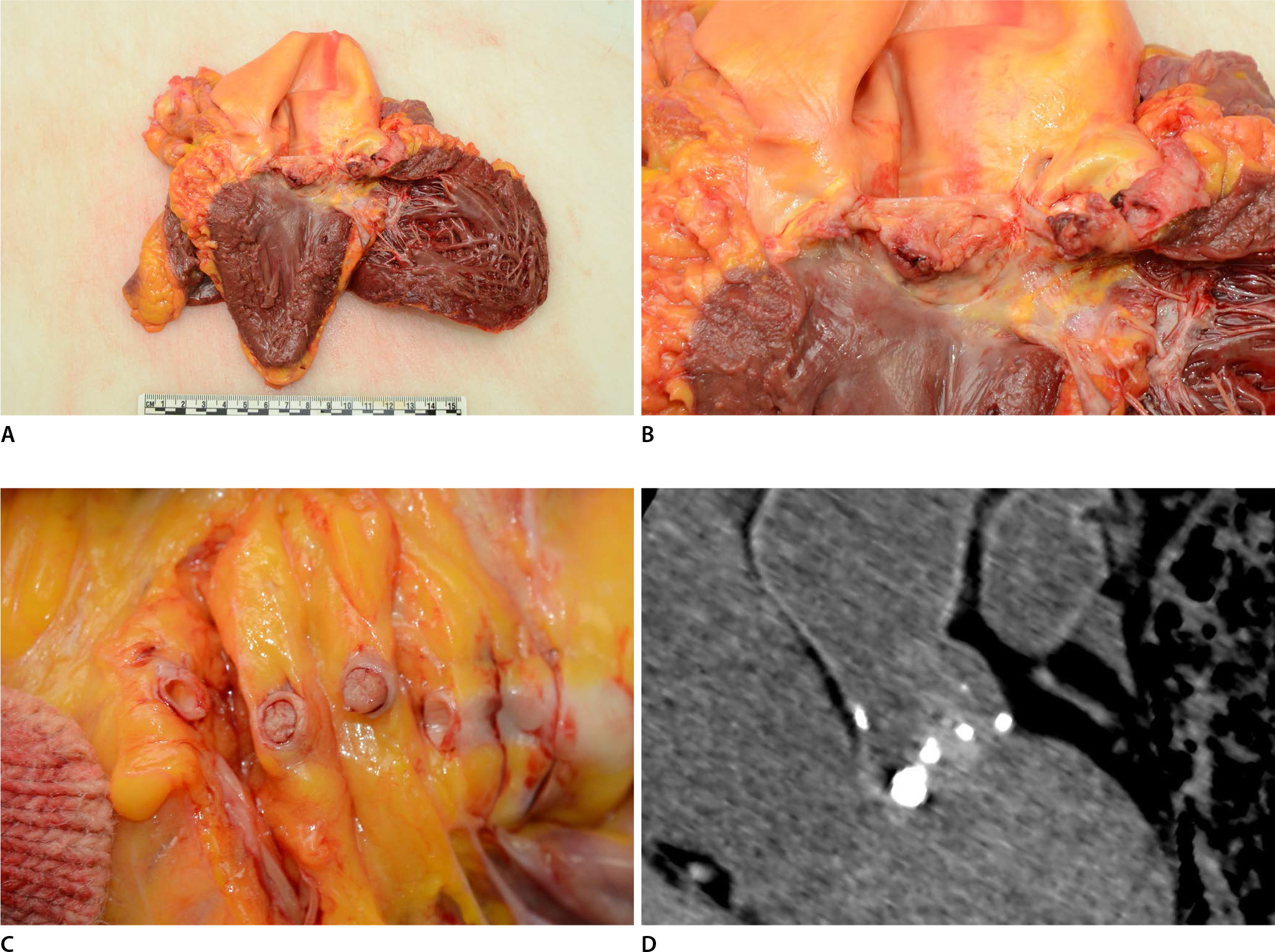
2.Na JY, Cho WY, Park JW, et al. Infective endocarditis: an autopsy case report with literature review. Korean J Leg Med 2014;38:78-82.

3.Dolinak D, Matshes E, Lew EOForensic pathology: principles and practice. Amsterdam: Elsevier Academic Press; 2005. p. 72-6.
4.Manzano MC, Vilacosta I, San Roman JA, et al. Acute coronary syndrome in infective endocarditis. Rev Esp Cardiol 2007;60:24-31.


5.Tiurin VP, Korneev NV. The mechanisms of the development and diagnosis of myocardial infarct in septic endocarditis. Ter Arkh 1992;64:55-8.
7.Thuny F, Avierinos JF, Tribouilloy C, et al. Impact of cerebrovascular complications on mortality and neurologic outcome during infective endocarditis: a prospective multicentre study. Eur Heart J 2007;28:1155-61.


8.Fabri J Jr, Issa VS, Pomerantzeff PM, et al. Time-related distribution, risk factors and prognostic influence of embolism in patients with left-sided infective endocarditis. Int J Cardiol 2006;110:334-9.


9.Brunson JG. Coronary embolism in bacterial endocarditis. Am J Pathol 1953;29:689-701.


10.Taherkhani M, Haybar H, Khaheshi I, et al. A rare case of acute myocardial infarction (AMI) due to infective endocarditis: clinical case presentation. J Indian Coll Cardiol 2015;5:160-3.

12.Burke A, Tavora FPractical cardiovascular pathology. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. p. 349-63.
13.Chan KL, Dumesnil JG, Cujec B, et al. A randomized trial of aspirin on the risk of embolic events in patients with infective endocarditis. J Am Coll Cardiol 2003;42:775-80.


14.Hunter AJ, Girard DE. Thrombolytics in infectious endocarditis associated myocardial infarction. J Emerg Med 2001;21:401-6.


16.Thuny F, Di Salvo G, Belliard O, et al. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation 2005;112:69-75.


17.Vilacosta I, Graupner C, San Roman JA, et al. Risk of embolization after institution of antibiotic therapy for infective endocarditis. J Am Coll Cardiol 2002;39:1489-95.


19.Glazier JJ. Interventional treatment of septic coronary embolism: sailing into uncharted and dangerous waters. J Interv Cardiol 2002;15:305-7.